
30+ Egg Freezing Statistics
Explore egg-freezing statistics and trends that offer valuable insights into the dynamic landscape of fertility preservation.

President of Florida Healthcare Insurance

Founder & Therapist of Uncover Mental Health Counseling
The United States is facing an ongoing healthcare crisis. Over 60% of Americans have one chronic disease, while 40% have two or more, with this number estimated to increase by 99.5% by 2050.
Living with chronic illnesses drastically changes a person’s quality of life, as they require long-term management. For employees, this means making regular doctor’s appointments, taking medications, and countless lifestyle changes.
However, the fragmented nature of our healthcare systems and limited physician visits make it challenging for patients to receive the care they need.
Implementing chronic care management (CCM) is a solution to bridging this gap and optimizing health outcomes.
In this article, we explore how chronic care management benefits employees and the entire organization by reducing overall healthcare costs and improving the quality and delivery of care to patients with chronic illnesses.
So, what is chronic care management?
CCM is a Medicare service that goes beyond traditional healthcare to support people with multiple chronic conditions, such as diabetes, hypertension, or arthritis.
Typically, CCM uses a team-based approach involving a doctor, nurse, care manager, and other healthcare professionals. These teams coordinate and work together to improve employees’ quality of life and reduce the risk of complications by offering regular check-ins.
The services offered are performed outside regular office visits, including email and phone consultations and remote patient monitoring.
For employees, this means staying on top of their care without constantly visiting a doctor’s office.
Ultimately, chronic care management aims to solve employees’ two pain points: improve health outcomes and provide access to a healthcare team that can take a whole-person approach to their needs.
Although it’s clear that chronic care management benefits employees with chronic illnesses in the workplace, it’s important to clarify what conditions qualify for chronic care management.
Employees must first be diagnosed with at least two chronic conditions to qualify for chronic care management. By definition, chronic conditions are long-term medical issues that aren’t easily cured and are expected to persist throughout their lives.
Some examples on the chronic care management diagnosis list include:
It’s important to note that CCM is not limited to these illnesses, and numerous other conditions also qualify.
But how great is the burden of these lifelong illnesses?
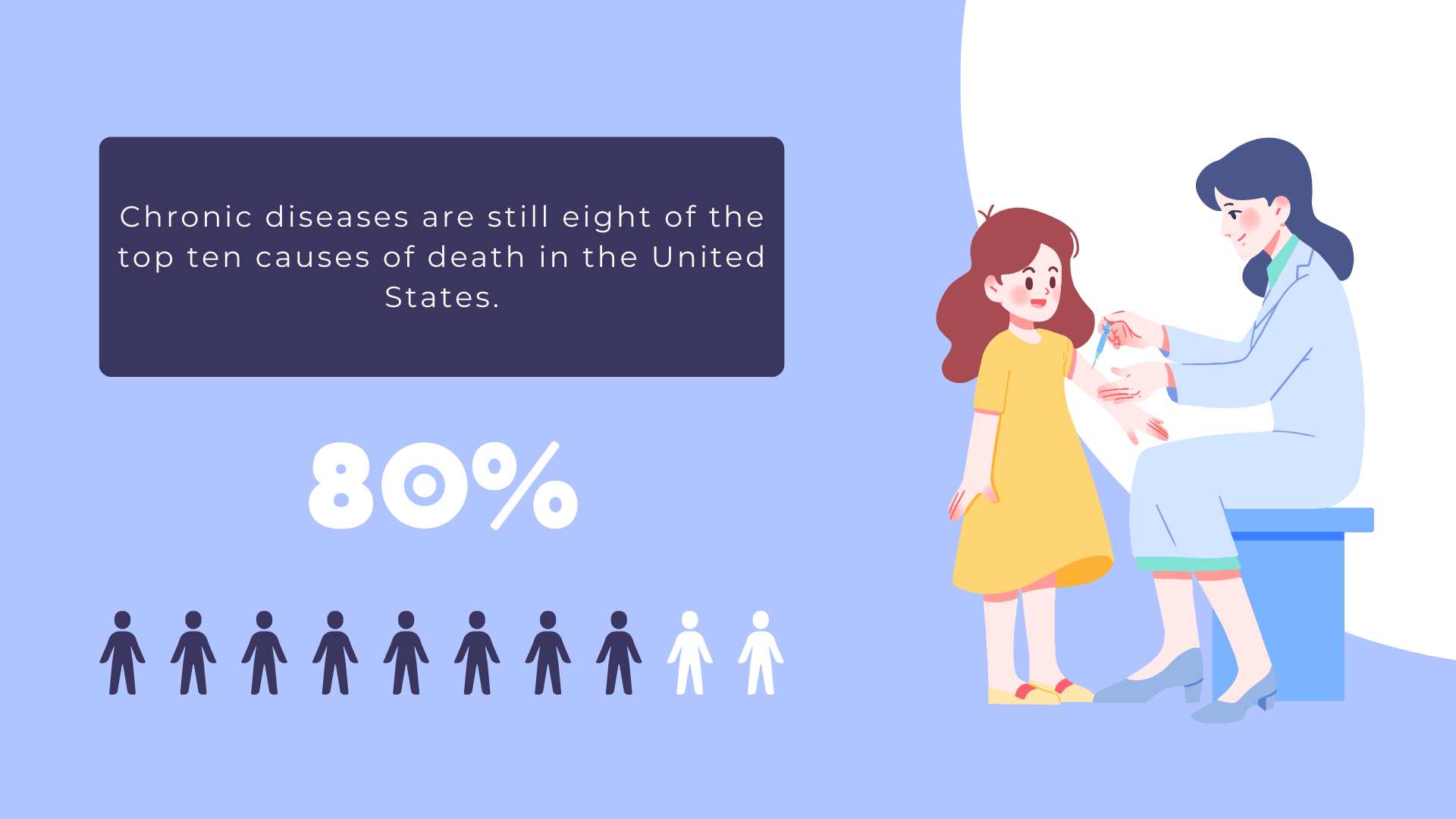
In recent years, the American lifespan has declined, partly due to COVID-19 and the rise in diseases of despair, including overdoses, suicides, and excessive alcohol use.
Despite these worrisome trends, chronic diseases are still eight of the top ten causes of death in the United States.
According to the CDC, chronic disease is the leading cause of illness, disability, and death, as well as a leading driver of the $4.5 trillion in annual healthcare costs in the US.
Typically, employees with several chronic conditions rely on a larger network of healthcare providers and are prescribed more medications, which raises their chances of hospitalization and care gaps due to the poor coordination of their treatment.
For these reasons, chronic disease patients have higher healthcare utilization and use healthcare services at more than twice the rate of those without such conditions. Inpatient utilization alone can be up to four times higher.
However, higher utilization leads to higher costs and increased financial strain.
For commercially insured employees with at least one chronic disease, average annual healthcare spending increases to approximately $8,900 per person, compared to just $1,700 for those without chronic conditions.
For employees with multiple chronic conditions, costs rise even more, regardless of the type of insurance.
Chronic care management has emerged as a potential solution and is transforming how we tackle these challenges.
Efforts to address health issues have primarily focused on disease prevention programs, which may not be as effective once an employee is dealing with multiple chronic conditions.
As the healthcare industry is transitioning to value-based care models, a growing emphasis is on proactive management of chronic conditions.
The good news is that most chronic diseases can be prevented and managed through healthy eating, regular physical activity, avoiding tobacco, and routine health screenings—all achievable through participation in chronic condition programs.
In addition to prevention, there are many other benefits of chronic care management.
One of the biggest benefits of CCM is that it gives employees personalized attention from a provider who knows their health conditions and actively helps them stay healthy.
Employees will start receiving CCM services only after an initial face-to-face doctor’s visit and consent to participate in these services.
Following the initial visit, those enrolled in a CCM program will receive a personalized care plan based on their health issues. A care plan could include:
Studies have shown that patients find these personalized care plans beneficial because they provide a clear roadmap for managing their health, consolidate important medical information, and help coordinate care across different providers.
How often have you had a health concern but felt that visiting the doctor’s office was too much of a hassle? For those with complex medical conditions, this is a common struggle.
CCM gives employees 24/7 access to physicians and clinical staff to address concerns, potentially avoiding unnecessary costs or hospitalizations.
Research shows that those enrolled in these services, previously hesitant to reach out for fear of burdening their doctors, now feel more at ease knowing someone is readily available to help and can connect them with their doctor if needed.
CCM focuses on meeting patients’ needs promptly, reducing worsening conditions, and avoiding costly ER visits and hospitalizations.
President of Florida Healthcare Insurance, Evan Tunis, highlights the significant advantages of CCM, stating, “Chronic care management benefits can provide significant advantages for employers, including improving employee health outcomes and reducing overall healthcare costs.“
Providers play a crucial role in chronic care management. Namely, they handle communication and coordination among the various healthcare professionals involved in a patient’s care.
Since CCM is a Medicare billable service, only qualified providers can include it in their monthly billing. Medicare requires that all CCM activities be supervised by a:
With a multidisciplinary team that includes physicians, nurses, care navigators, and others, employees benefit from a more unified and thorough approach to their health.
These teams—whether core, coordinating, or contingency —work together to create the care plan, manage medications, coordinate referrals, and offer patient education.
As a result of this collaboration, care fragmentation is reduced, the risk of medical errors is lower, and healthcare resources are better utilized.
Health equity and access are critical components of chronic care management. With CCM, employers can ensure that all employees receive the care they need regardless of their background.
By addressing social determinants of health, such as socioeconomic status, geography, and cultural barriers, CCM programs can help reduce disparities in healthcare.
With this approach, employees experience better health outcomes and fosters a more inclusive and productive workplace.
Through tailored care plans and proactive management, CCM helps bridge the gap, offering equitable healthcare access.
One of the most pressing challenges in today’s business world is trying to find ways to reduce healthcare costs for employers.
A survey by the Advisory Board and UnitedHealthcare found that 60% of employers want improved care management for costly conditions, while 55% prioritize early identification and treatment.
In the United States, 90% of the $3.5 trillion spent annually on healthcare is directed towards those with chronic and mental health conditions, which are the primary drivers of healthcare costs.
Beyond these direct expenses, there are many hidden costs due to absenteeism and productivity loss, totaling up to $36.4 billion in lost workdays.
Chronic Care Management (CCM) programs have been shown in studies to significantly lower annual healthcare expenses through the following benefits:
In fact, Medicare data indicates that CCM can reduce unnecessary hospital visits by at least 4.7% and emergency department visits by 2.3%.
Introducing chronic care management programs in the workplace requires careful consideration of both regulatory and financial aspects.
On the regulatory side, compliance with healthcare laws such as the Health Insurance Portability and Accountability Act (HIPAA) is crucial to ensure the privacy and security of patient data.
On top of that, employers must also navigate state-specific regulations, especially if they offer CCM services through employer-sponsored health plans.
Financially, introducing CCM benefits can be a strategic investment for employers.
As shown before, companies could potentially reduce overall healthcare costs by improving the management of chronic conditions among employees.
On the other hand, employers must consider the costs associated with setting up and maintaining CCM programs, including software investments and potential partnerships with external healthcare providers.
However, the long-term savings achieved through better health outcomes and reduced absenteeism may offset these costs, making CCM a financially smart option for many organizations.
Many people may wonder, “How much does Medicare pay for chronic care management?”
Medicare Part B covers chronic care management (CCM) services but only pays for 80% of the total cost.
In other words, patients are responsible for the remaining 20% of the bill, which is typically billed as a copay.
However, those with supplemental insurance like Medigap, or dually enrolled in both Medicare and Medicaid, may not have to pay this out-of-pocket expense.
In such cases, the remaining 20% is usually covered by their additional insurance.
As chronic conditions rise, employers must decide to implement chronic care management programs or face increasing healthcare costs and productivity losses.
Chronic care management benefits employees and organizations by reducing the impact of conditions like diabetes in the workplace, heart disease, and common work-related musculoskeletal disorders.
Kristie Tse, Founder & Therapist of Uncover Mental Health Counseling, emphasizes the importance of these initiatives, stating, “Creating a culture of wellness not only fosters better health but also enhances productivity. For example, I often see clients struggling with chronic conditions who benefit from coordinated care efforts that include regular monitoring, personalized management plans, and access to mental health resources.”
Ultimately, prioritizing chronic care management is not just a choice—it’s a strategic decision that ensures both healthier employees and a more resilient organization.
Disclosure: Some of the products featured in this blog post may come from our partners who compensate us. This might influence the selection of products we feature and their placement and presentation on the page. However, it does not impact our evaluations; our opinions are our own. The information provided in this post is for general informational purposes only.
Senior Content Writer at Shortlister
Browse our curated list of vendors to find the best solution for your needs.
Subscribe to our newsletter for the latest trends, expert tips, and workplace insights!

Explore egg-freezing statistics and trends that offer valuable insights into the dynamic landscape of fertility preservation.

How can organizations and patients adapt to the shift toward consumer-centric pricing transparency?
Chronic disease management provides a dual advantage in the workplace, supporting employee health and organizational success. Learn how you can implement the right program for your company.

As a healthy workforce represents a healthy society and vice versa, it’s paramount for cardiovascular disease prevention to find its place in the workplace.
Used by most of the top employee benefits consultants in the US, Shortlister is where you can find, research and select HR and benefits vendors for your clients.
Shortlister helps you reach your ideal prospects. Claim your free account to control your message and receive employer, consultant and health plan leads.