
What is Pharmacy Benefit Management (PBM)?
If two different people with the same prescription medicine get two different bills for the same medicine, it makes you wonder – how is the price of the prescription medicine determined?

CEO, Edstellar
Every day, millions of employees face the (often) invisible struggles of chronic diseases. For some, it could be coping with a flare-up or managing symptoms in a high-pressure environment. For others, it could be caring for an affected family member while meeting tight deadlines.
This dual burden goes beyond personal impact and profoundly affects workplace dynamics, productivity, and morale.
Chronic disease management emerges as a solution for both.
On one hand, it can significantly ease the strain on workers, providing them with resources to manage their health or caregiving responsibilities. On the other hand, it helps companies mitigate productivity losses and associated costs.
However, its implementation is a multiple-step process that involves everything from assessing workplace needs and choosing the right approach to considering legal and ethical concerns and addressing health equity.
Below, we offer a comprehensive analysis of each these aspects.
To begin, what is chronic disease management?
Chronic disease management involves the ongoing care and support for those with long-term health conditions such as diabetes, heart conditions, arthritis, and asthma. It’s an integrated approach that combines monitoring, treatment, lifestyle changes, and preventative measures to control symptoms, slow disease progression, and improve the patient’s quality of life.
In the workplace, the importance of chronic disease management extends beyond employee health, demonstrating how a strategic approach to well-being can strengthen organizational resilience and improve employee performance.
What are chronic conditions?
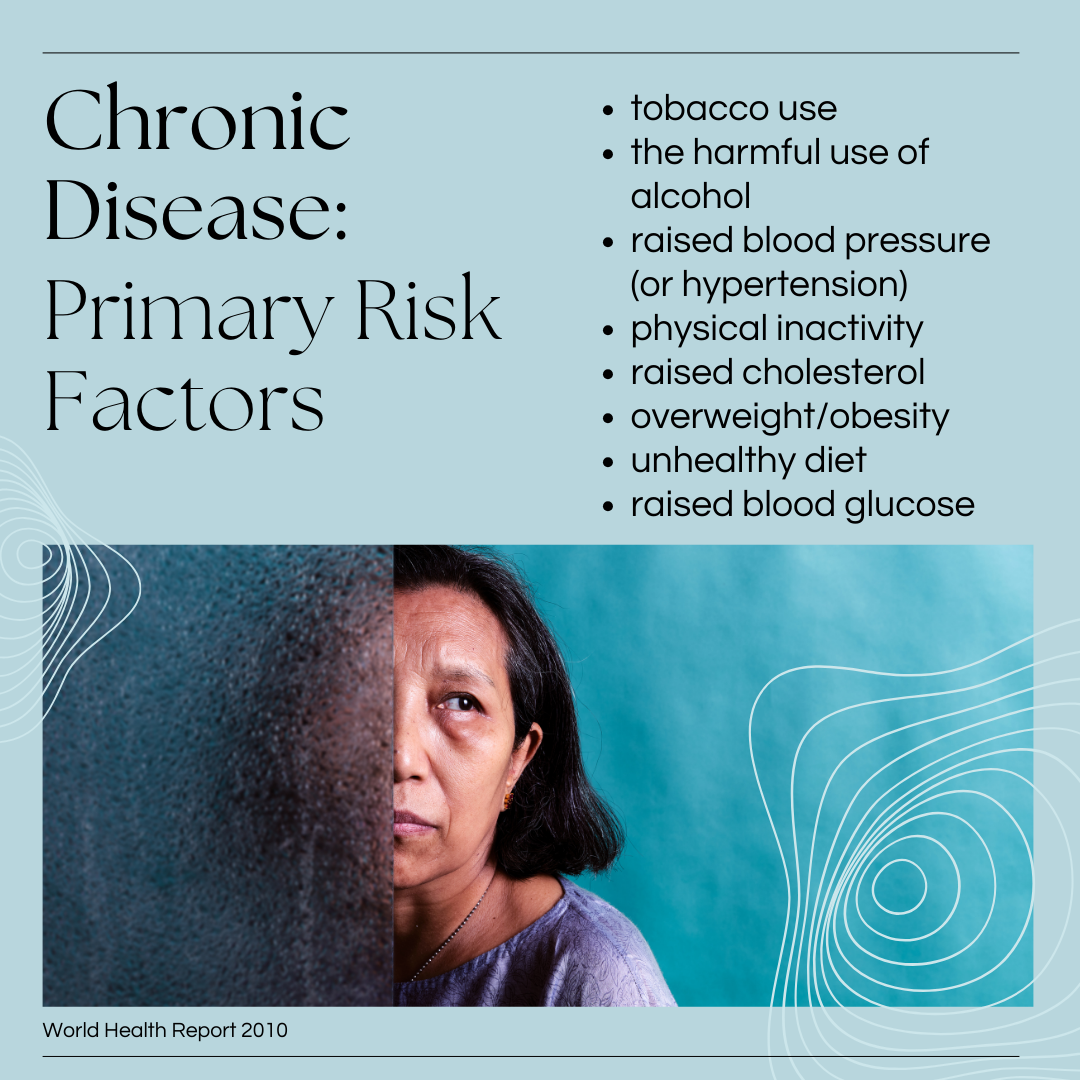
The CDC defines chronic diseases as “conditions that last one year or more and require ongoing medical attention or limit activities of daily living or both.”
What causes them?
This versatile categorization makes it challenging to determine a single cause. However, primary risk factors like smoking, poor nutrition, physical inactivity, and excessive alcohol use have been known to worsen them.
What’s their impact on the workplace?
As long-term issues that usually can’t be cured, they need proper support and care. Otherwise, they disrupt a person’s daily functioning in and out of the workplace, affecting productivity and efficiency, impacting their social life, increasing stress, and causing financial strains.
The severity of this becomes more evident if we consider that one-third of workers are affected by at least one chronic condition, while 11% deal with multiple.
Another 35% are also caregivers for family members with chronic conditions.
Recognizing the extent of these challenges calls for a supportive work environment where reasonable accommodation is more than a nice-to-have perk.
However, the “how” in implementing chronic disease management in the workplace depends on multiple factors, including a better understanding of these conditions, their extent, and how to address them.
While these are the most common examples, many chronic conditions often go unnoticed despite their severity, from allergies and asthma to high blood pressure and mental health disorders.
Musculoskeletal disorders are another pain point, especially those directly caused or influenced by workplace factors. For example, repetitive movement, awkward postures, or excessive force can lead to or worsen tendinitis, while poor ergonomics and prolonged periods of sitting can contribute to chronic lower back pain.
Having outlined the chronic diseases that frequently challenge today’s workers, we now focus on potential solutions.
Enter occupational health.
According to the World Health Organization, occupational health is “an area of work in public health to promote and maintain the highest degree of physical, mental, and social well-being of workers in all occupations.” It combines several disciplines, including medicine, ergonomics, and psychology – all valuable aspects of managing chronic conditions.
Chronic condition programs fall under the umbrella of occupational health.
They are specifically designed to identify and manage the risks and symptoms associated with these diseases, from health screenings and monitoring, support, and rehabilitation to ergonomic assessments and reasonable accommodation. They can also integrate proactive measures such as flexible work arrangements, education, training, and employee support.
Beyond health implications, the relationship between these programs and the workplace reveals a broader impact on organizations, their efficiency, and overall success.
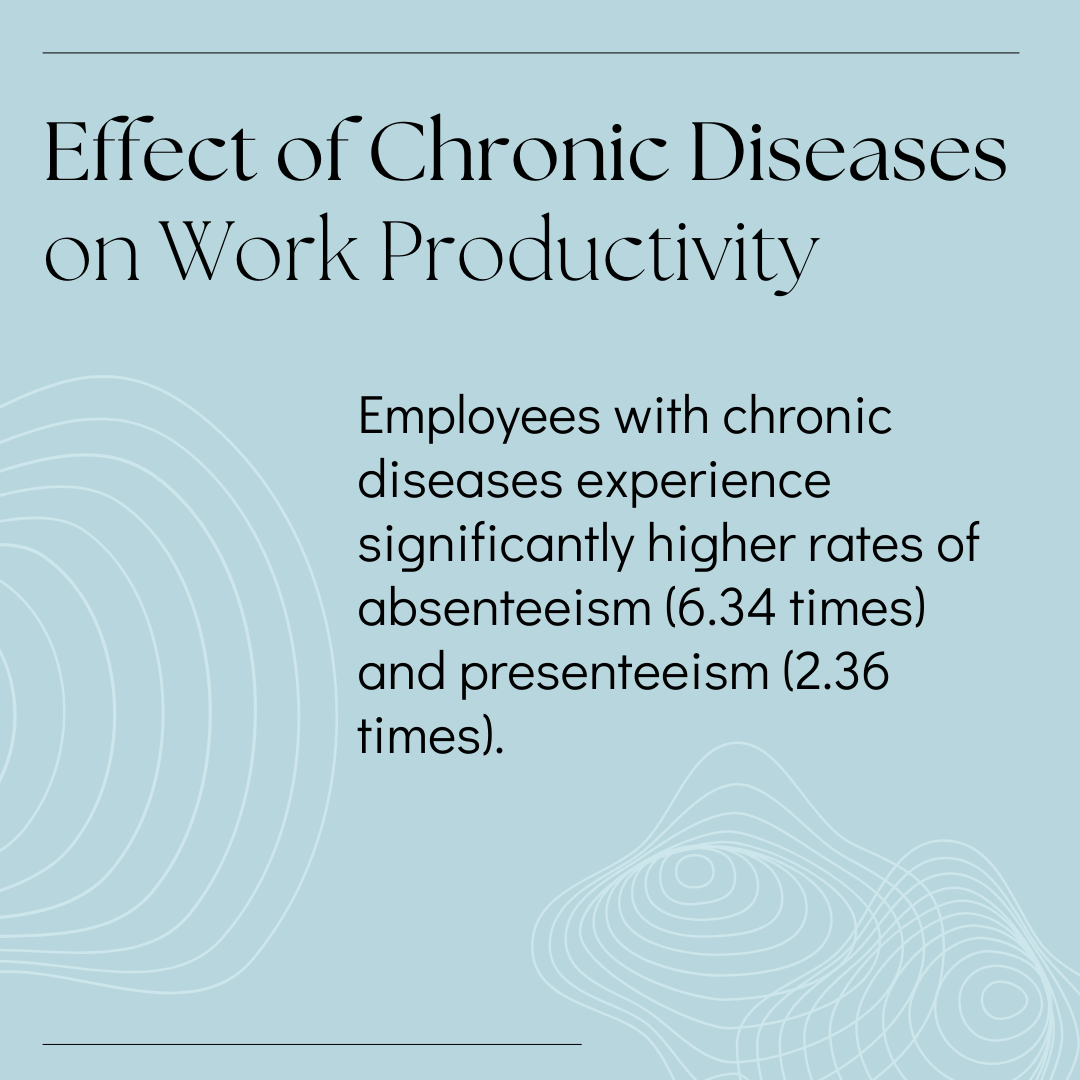
A study titled Effect of Chronic Diseases on Work Productivity: A Propensity Score Analysis found that employees with chronic diseases experience significantly higher rates of absenteeism (6.34 times) and presenteeism (2.36 times) than those without chronic conditions.
The effects were even more pronounced in individuals with multiple conditions.
In fact, different chronic condition combinations have a distinct impact on missed workdays. Namely, adults with arthritis, diabetes, and heart disease experienced the highest average absenteeism, or 14.42 days to be exact. In comparison, combinations like hypertension and diabetes in the workplace lead to fewer missed days.
The financial impact of this amounts to trillions of dollars.
In fact, the health and economic costs of chronic conditions and mental health disorders account for 90% of the nation’s $4.5 trillion in annual healthcare expenditures.
Heart diseases alone cost the healthcare system $254 billion per year and companies $168 billion in lost productivity, while diabetes costs another $413 billion in combined expenses.
This massive financial burden highlights the apparent efficacy of implementing chronic disease management programs that address one or more conditions.
After weighing the impact on health, productivity, quality of life, and the overall cost of chronic illness, it’s easy to see the direct benefit of effective chronic condition management.
For employees, access to such programs can lead to greater disease control, less stress in their daily lives, and better health outcomes. At the same time, knowing their employer supports them could improve their job satisfaction and influence their career longevity since disease management can help them stay efficient.
For employers, all these employee benefits translate to better productivity, lower absenteeism, and presenteeism. Additionally, proactively managing chronic conditions can affect the frequency and severity of medical interventions, which, in turn, could reduce healthcare costs for employers.
Despite these programs’ generally positive impact, key considerations remain to consider during their implementation.
Implementing a chronic disease program involves ethical concerns, as it is a sensitive matter that can quickly turn biased.
For starters, confidentiality is vital, requiring employees’ medical information (collected and used with informed consent) to be protected and used solely for its intended purpose. Participation in these programs should be voluntary, and respecting employee autonomy means offering support without pressuring them into specific health behaviors.
From a legal standpoint, compliance and the protection of employee rights appear as focal points.
Under the Americans with Disabilities Act (ADA), employers must provide reasonable accommodations for employees with disabilities, including chronic health conditions. Programs must align with ADA requirements to avoid legal issues. This act also protects employees against discrimination based on their disability.
At the same time, the Family and Medical Leave Act (FMLA) provides eligible employees with the right to take unpaid leave for medical reasons without sacrificing their job security.
Like the ADA, this law ensures that employees are treated fairly in the workplace, regardless of their health conditions.
A study on living with chronic disease and the views of patients reveals that sadness and worry are the most common emotions. Changes in their life were marked as predominantly negative, especially in managing work, while the study identified friends, family, and healthcare professionals as the biggest support. Work was also recognized as “supportive,” along with leisure-time activities, beliefs, hope, and religion.
Since work plays a significant role in a person’s life, employers become critical to supporting workers. Even more so, considering that an organized approach to managing complex and often unpredictable health conditions can make a significant difference.
The following steps outline how to manage chronic diseases in the workplace, highlighting the importance of companies as another valuable source of support.
The first step is understanding the specific health challenges within the organization. Companies can use surveys, review health claims data, and consult with HR or benefits managers to establish a focused approach to chronic disease management. Since it’s a sensitive matter that employees may not want to discuss openly, companies should ensure confidentiality.
Involving different perspectives can guarantee the program is inclusive and practical. Bringing together key stakeholders, including leadership, management, and employees, should support a more straightforward implementation. It’s also important to engage healthcare providers and benefits coordinators to ensure the necessary resources are in place.
Once you’ve gathered data and included all necessary parties, it’s time to develop an action plan. This step ensures all company policies and procedures reflect the previous two.
Depending on the specific needs of the affected employees, this may include everything from flexible work arrangements and clear leave policies to easy access to healthcare resources and comprehensive benefit programs.
Clear communication is as necessary in this stage as it is in the others, ensuring that employees know their rights and have easy access to support and resources.
Workplace accommodations for employees with chronic conditions are a broad category. For example, ergonomic equipment like adjustable chairs or specialized keyboards can be an excellent solution for common work-related musculoskeletal disorders like arthritis or Carpal Tunnel Syndrome. Assistive technology can help employees with visual impairments or hearing loss, while a more flexible schedule or extra breaks can help employees with lower energy levels or pain flare-ups.
Make sure to tailor accommodations to employees’ needs without them feeling excluded or stigmatized.
Finally, no program is complete without regular monitoring and evaluation.
“Employers should monitor key performance indicators like fewer absences, lower healthcare costs, and higher employee productivity to see how well and how much chronic disease management programs are helping.
By conducting regular health checks, staff surveys, and looking at patterns of healthcare use, data can be gathered about how well a program is working”, comments Arvind Rongala, CEO of Edstellar.
“Monitoring changes in employees’ health, such as fewer signs of illness or better control of long-term conditions, is another way to see how the program is working.
Regular reviews and adjustments based on these metrics help the program work better and show the company how valuable it is,” Rongala concludes.
Now that we understand the technical process of managing these diseases, let’s circle back to what matters most: the people.
Accommodation is one part of the equation.
However, the other equally important part is support.
According to Managing People with Chronic Diseases in the Work Environment: A Practical Guide for Companies and Employers, this support, in the form of health promotion, can include aspects linked to employees’ physical, psychological, and social well-being.
The guide mentions the following examples:
This means implementing targeted solutions depending on the kind of support employees need.
“Employers can run successful programs for managing chronic diseases by combining thorough health screenings with individualized care plans,” suggests Arvind Rongala.
“Offering wellness rewards, on-site or virtual health coaching, and making it easier for people to get the medicines they need are all very important.”
Rongala goes on to say that “creating a supportive atmosphere by teaching employees how to deal with chronic diseases and promoting a health-conscious culture can make them much more engaged.”
“Making sure that workers can access mental health resources and tools for dealing with stress is also good for their physical health and makes the program work better as a whole,” he concludes.
In summary, this translates into several strategies companies can use for employee support.
EAPs address many of the aspects above, especially surrounding mental wellness and social wellness, alcohol and substance abuse, stress, etc. Depending on the EAP provider, they also work with managers and supervisors to offer the correct solutions for organizational challenges related to chronic disease management.
Mental health and wellness are top priorities when dealing with chronic illness in the workplace. They directly affect prevention and disease management, best seen when companies adopt a holistic approach targeting various physical and mental health factors.
Workplace wellness trends for 2024 show employers are increasingly tailoring employee benefits and wellness programs to address specific needs and challenges. Expectedly, the report shows how the pandemic increased interest in mental health providers, which plays a significant part in dealing with the effect of chronic conditions on employees’ emotional states.
As part of the holistic approach to wellness, there has also been an increase in chronic condition programs, weight management programs, corporate sleep programs, diabetes programs, corporate musculoskeletal programs, etc.
Many of these already have or are expanding to include remote options, allowing employees to access support and resources from anywhere.
Addressing immediate factors that can cause or worsen chronic conditions helps mitigate flare-ups and manage symptoms more effectively.
However, health coaching and chronic disease education offer tailored guidance and support for long-term results.
While the former focuses on setting achievable goals and sticking to the plan, chronic disease education provides a well-rounded understanding of the specific condition for and beyond the affected employees. It can promote learning, increase awareness, and even build empathy, challenging potential biases and stigma in the workplace.
A study exploring health equity gaps in state chronic disease prevention sheds light on how these efforts address (or fail to address) health disparities.
While awareness of health equity has increased, its integration into practice remains inconsistent.
According to the analysis, addressing health equity in chronic disease management requires a multifaceted approach:
In the context of workplace disease prevention programs, this means ensuring equal access to resources and support for all employees. Employers should also focus on understanding and mitigating the social determinants of health contributing to chronic conditions and incorporate equity-focused strategies into workplace health initiatives.
Looking ahead, companies will likely continue adopting value-based care models. These models focus on long-term health and coordinated care, helping to reduce expensive medical treatments and boost overall well-being.
Remote care is also gaining momentum, showing that it isn’t just a backup but a powerful tool for greater accessibility.
We’re also shifting towards more personalized care, where programs are tailored to fit individual needs and circumstances. This makes it easier for employees to manage their conditions in and out of the workplace.
All these trends are moving us towards a future where chronic disease management programs are more supportive, accessible, and practical, leading to a healthier and more productive workforce.
Disclosure: Some of the products featured in this blog post may come from our partners who compensate us. This might influence the selection of products we feature and their placement and presentation on the page. However, it does not impact our evaluations; our opinions are our own. The information provided in this post is for general informational purposes only.
Content Writer at Shortlister
Browse our curated list of vendors to find the best solution for your needs.
Subscribe to our newsletter for the latest trends, expert tips, and workplace insights!

If two different people with the same prescription medicine get two different bills for the same medicine, it makes you wonder – how is the price of the prescription medicine determined?
As heart disease and work stress are closely linked, the question remains: Can the stress caused by work be so severe that it causes a heart attack?
To what extent do breast cancer patients struggle with financial toxicity while battling this illness? What factors contribute to this financial toxicity?
These vital men’s health statistics depict the importance of addressing men’s health issues and promoting holistic approaches to men’s healthcare.
Used by most of the top employee benefits consultants in the US, Shortlister is where you can find, research and select HR and benefits vendors for your clients.
Shortlister helps you reach your ideal prospects. Claim your free account to control your message and receive employer, consultant and health plan leads.