In their 2022 Employer Health Benefits Survey, KFF revealed that telemedicine benefits in the workplace dramatically increased during lockdown.
Among businesses with 50 or more employees offering health benefits, 87% of small and 96% of large firms included telemedicine in their health plans.
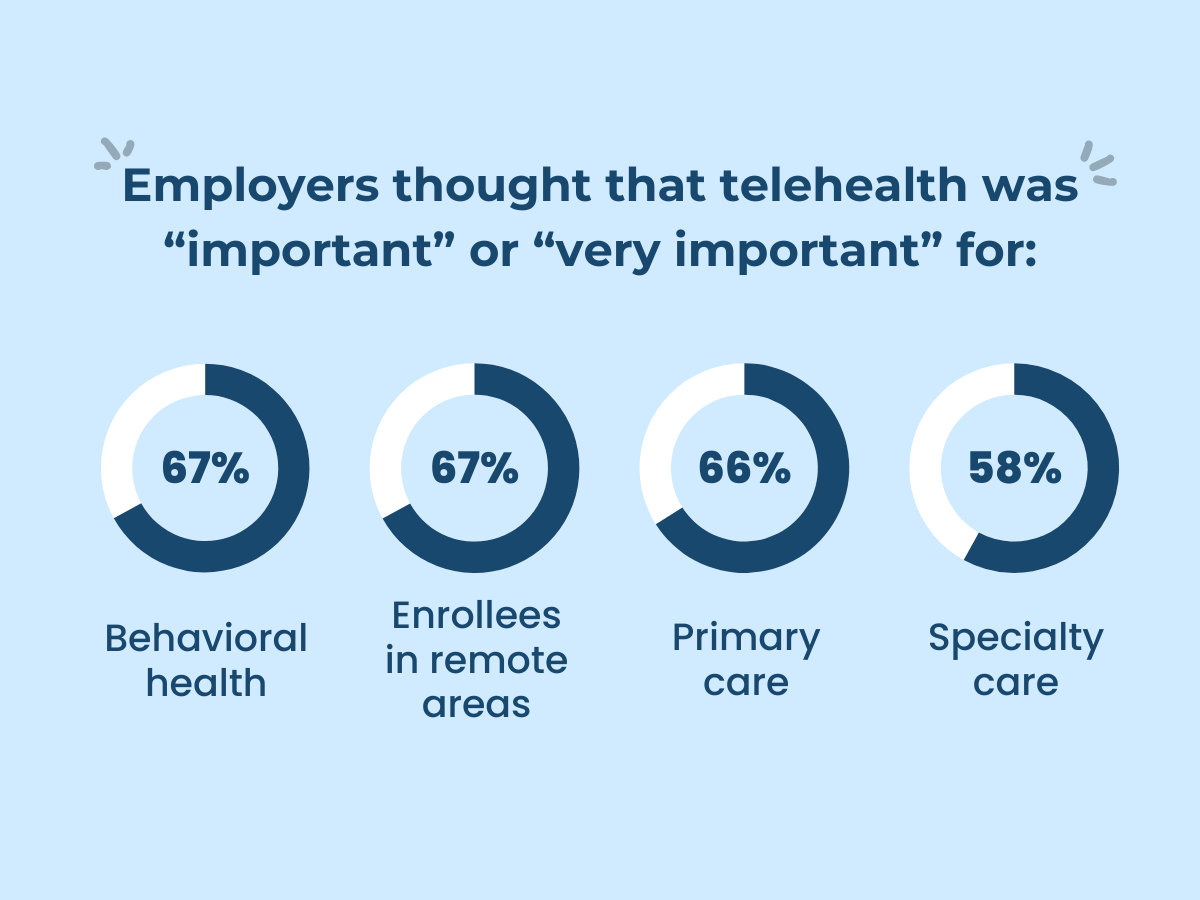
Moreover, when asked about its future importance, employers thought that telehealth was “important” or “very important” for:
- Behavioral health – 67%
- Primary care – 66%
- Specialty care – 58%
- Enrollees in remote areas – 67%
Recognizing its significance and growth post-pandemic, it begs the question: how did this transformation in healthcare unfold?
A quick look at the past reveals a substantial shift in not only how healthcare is delivered but also how it’s managed and experienced today.
Take, for example, medicine and medical practice.
Before the pharmaceutical industry, people used home remedies, mainly relying on a trial-and-error approach. Medical practice was largely reactionary, with limited diagnostic tools and treatments, which made many nonlife-threatening illnesses today a death sentence in the past.
In contrast, modern medicine, supported by technological advancement and scientific breakthroughs, introduced new medications, medical equipment and facilities, and life-saving treatments. In line with this, the number of practicing doctors surged by more than 400%, going from 219,900 in the 1950s to over 1.1 million as of January 2024 in the US alone.
Then came health information technology, big data, augmented reality, and artificial intelligence.
These pushed healthcare towards a more patient-centered and data-driven model, improving access to quality care. In addition, the COVID-19 pandemic accelerated the adoption of virtual care, including doctor-on-demand, remote patient monitoring, and virtual consultations.
Beyond addressing physical health concerns, these were crucial in supporting employees’ mental well-being during times of heightened stress and uncertainty. They expanded access, improved cost control, and ensured better health for the workforce, fortifying their importance as part of the modern healthcare system while challenging the traditional ways of accessing care.
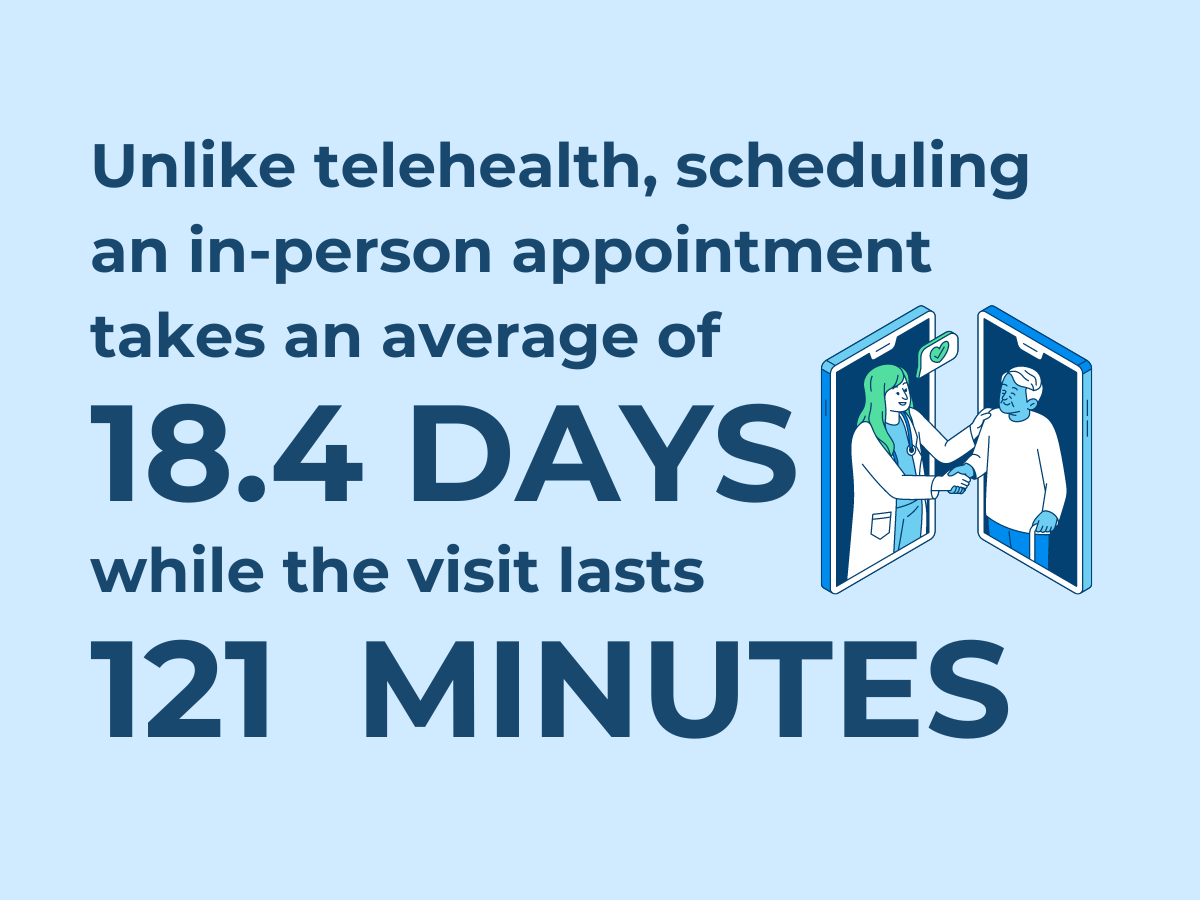
Yet, despite all of this, the hands-on approach retained its significance.
As we set the ground for the telehealth vs. in-person care discussion, let’s first examine where these two fit within the healthcare system.