50+ Infertility Statistics
Discover 50+ essential infertility statistics and get valuable insights into this prevalent issue.
Does telehealth reduce costs? As healthcare evolves in the digital age, this question has become increasingly relevant.
With the rise of virtual medical services, patients and employers alike are discovering that telehealth services not only offer convenience and accessibility but could also potentially lower healthcare expenses.
In this article, we explore the world of telehealth, its history, benefits, and the compelling evidence that suggests it may be the key to more affordable and equitable healthcare for all.
In simple terms, telehealth involves using technology that allows medical services to be received remotely without an in-person visit with a doctor. Telehealth is often available through secure apps and websites and may use different communication channels such as:
A telehealth appointment is similar to a traditional doctor’s visit. Although patients don’t meet the healthcare provider face-to-face, they can still discuss their symptoms, receive medical advice, and even get a prescription.
The concept of telehealth has existed for centuries.
In 1879, an article in the Lancet mentioned using the telephone to cut down on unnecessary office visits. By 1925, the cover of Science and Invention magazine featured a doctor diagnosing a patient via radio and even envisioned a device for video examinations from afar.
Surprisingly enough, it was NASA’s Mercury space program that really put into practice conducting physiological monitoring over long distances.
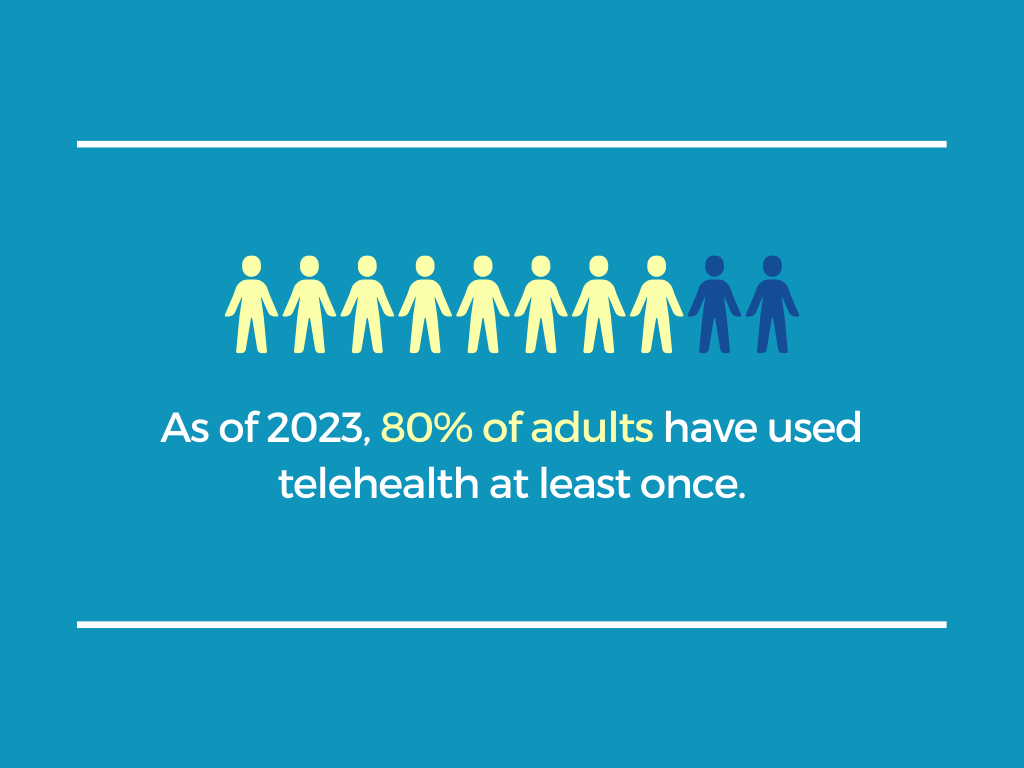
Today, because of technological advancements and updates made due to the COVID-19 pandemic, telehealth services have become more accessible than ever. As of 2023, 80% of adults have used telehealth at least once in their lives.
Generally, telehealth services fall into three main types:
Traditional healthcare costs can be broadly categorized into three main areas: direct costs, indirect costs, and administrative costs.
Each of these categories contributes to the overall expense of healthcare for employees and families, making healthcare affordability a major concern in many countries.
The direct costs category includes expenses directly associated with medical services, such as in-person consultations, hospital stays, surgeries, and treatments. As expected, these costs can be substantial, covering everything from physician fees to the use of medical facilities and equipment.
Indirect costs are all the expenses associated with seeking healthcare, such as travel to and from medical appointments, childcare, time taken off work, and the potential loss of income during recovery periods. These “hidden” costs can quickly add up, particularly for employees requiring frequent or prolonged treatment.
Administrative costs involve overhead expenses related to managing healthcare services. These include the costs of billing, scheduling appointments, maintaining patient records, and handling insurance claims.
Virtual services—such as telemedicine and Doctor on Demand—have traditionally been cheaper than “brick-and-mortar” visits.
But how does telehealth reduce costs, and what makes these services cheaper?
While there are many reasons, the simplest one is that resolving patient issues in a virtual setting eliminates costly travel expenses and visits to emergency rooms.
In the United States, where 6 million people live more than 30 minutes away from the nearest hospital, transportation remains one of the greatest barriers to healthcare, making it a major social determinant of health.
Virtual care not only removes barriers to getting timely help but also saves money on fuel, parking fees, and public transportation costs.
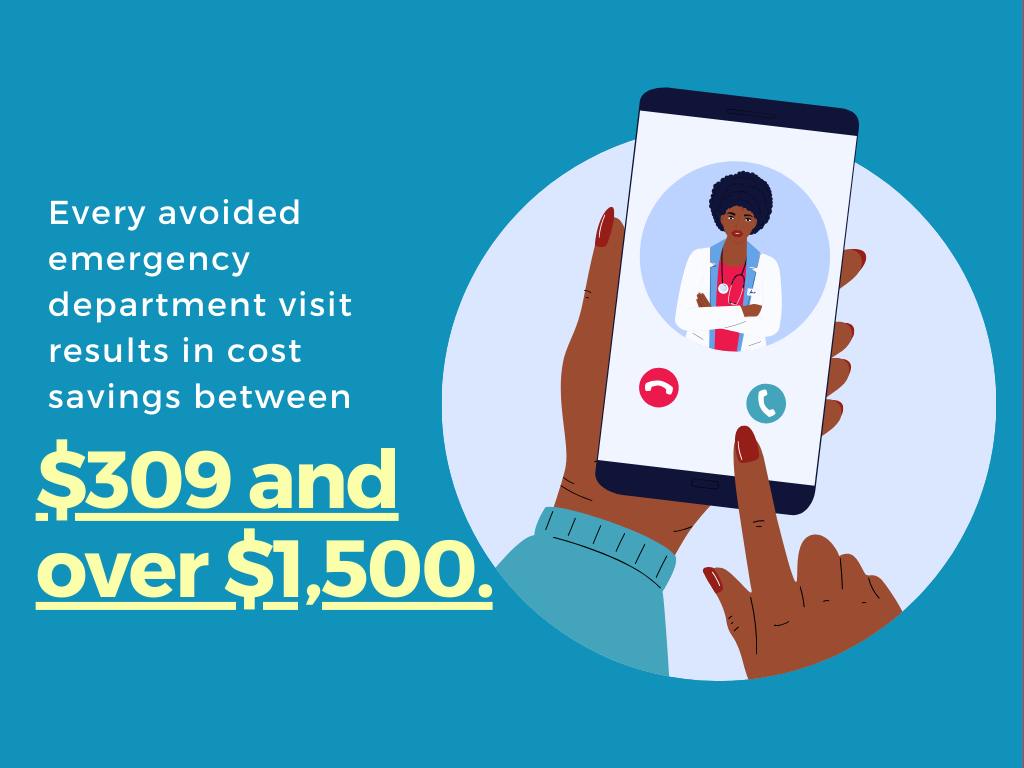
Another point is that redirecting care from the ER and urgent care facilities proves to be both cost-efficient and beneficial for the whole healthcare system.
Studies show telehealth prevents unnecessary hospitalizations and reduces the risk of overwhelming healthcare systems.
In fact, a study by Jefferson Health System found that every avoided emergency department visit resulted in cost savings between $309 and over $1,500.
Additionally, in-person healthcare visits often come with facility fees that can drive up the overall cost of care. Virtual care, on the other hand, lowers administrative costs by automating and digitizing many processes, further reducing expenses.
So, how does the cost of telehealth compare with traditional healthcare?
On average, a telehealth visit costs between $40 and $50, whereas an in-person visit costs more than double that, averaging around $176.
However, the telehealth cost savings extend beyond just these initial numbers.
In fact, a series of studies conducted by Veracity Analytics and Dr. Niteesh Choudhry of Harvard Medical School found that, on average, each telehealth visit results in cost savings of $518 to $717.
Surprisingly, the results consistently show that cost savings increase significantly in the month following the initial telehealth treatment.
It was shown that patients who use telehealth tend to seek care sooner for the same illness than those who visit other providers. As a result, they experience less severe conditions and have a reduced need for follow-up care.
Similarly, another study showed that telehealth is a more affordable option for virtual care without raising overall follow-up rates or antibiotic usage compared to urgent or primary care.
Given the compelling evidence from multiple studies, it’s clear that telehealth not only offers immediate cost savings but also contributes to long-term health and financial benefits.
While mental health consultations and prescription refills are often the first ideas that come to mind when we think of telehealth, the scope of this technology extends beyond these common applications.
Beyond behavioral health, telehealth has made significant inroads into numerous medical specialties, such as telestroke, teledermatology, and telecardiology.
As we explore real-world case studies and telemedicine statistics, it becomes evident that telehealth is revolutionizing the healthcare landscape.
Before the pandemic, the no-show rate for in-person psychiatry visits was 11%, but this rate fell to 6% after the shift to virtual visits. Another study showed that telepsychiatry services reduced the cost of mental health care by 38% compared to traditional in-person care.
Patients enrolled in a Digital Medicine program experienced better blood pressure control than those receiving usual care (79% vs. 26%). In addition, in the same study, primary care physicians saw a 29% decrease in clinic visits from participating patients, which helped decrease their workloads and allowed them to see more patients.
A systemic review of 21 telehealth studies showed that families saved between $36 and $357 on travel costs with online postoperative care. On average, patients saved about 2.25 hours in travel per appointment, meaning parents and children missed less work and school.
When analyzing well-photographed lesions, dermatologists identified nearly 10% more skin cancers and had 40% fewer referrals. Another 2020 study found that teledermatology reduced the wait time for in-person dermatology appointments by 78%.
In one study, women reported lower stress at both 14 and 36 weeks of gestation than those receiving standard care. According to another study, an alternative prenatal schedule supplemented with mobile technology and home monitoring led to a savings of $499.14 per pregnancy.

The intersection of healthcare and technology has never been more dynamic, with advancements driving significant changes in how care is accessed and delivered.
As employers strive to improve employee well-being and optimize healthcare benefits, telehealth has emerged as an innovative solution.
The virtual-first transformation of healthcare not only streamlines access to medical professionals, but also aligns with the modern workplace’s demands for flexibility, efficiency, and personalized care.
By adopting telehealth services into employee benefits packages, companies are discovering many advantages that benefit their workforce and their bottom line.
For employees, the convenience and accessibility of telehealth are hard to ignore.
The ability to connect with a doctor or therapist from anywhere, without the hassle of commuting or wasting precious time in a waiting room, is not just convenient but a time-saver that can make a world of difference in a busy day.
Knowing that quick advice on a nagging cough or persistent headache is just a call away can ease anxiety and improve patient experience.
In addition, personal time is not sacrificed for healthcare, contributing to a healthier work-life balance for workers, families, and caregivers.
For those managing chronic diseases or needing regular follow-ups, telehealth means continuity of care without the scheduling nightmares.
From an employer’s perspective, the benefits are equally compelling.
When employees can resolve health concerns quickly without leaving the office, it translates to greater productivity and fewer sick days. In simpler terms, they’re not out for half a day to attend a 15-minute appointment.
Financial benefits exist, too. Employers can reduce overall healthcare costs by making it easier for employees to get regular check-ups and early diagnosis and intervention.
Moreover, telehealth promotes equity in access to care. Not all employees have equal healthcare access due to location, scheduling constraints, or even mobility issues.
Telehealth bridges these gaps, ensuring everyone can access quality care, from the busy executive to the remote worker. For those in rural areas or underserved communities, telehealth can be a lifeline, connecting them with clinicians, specialists, or services that might otherwise be out of reach.
What was once considered a “nice-to-have” benefit is now a “must-have” for employers. In other words, telehealth is no longer an alternative healthcare model but a supplementary one to the traditional one.
Radish Health
Radish Health's expertise, emphasis on personalized care, comprehensive services, and commitment to patient satisfaction make it an excellent choice for a top telehealth solution. Visit Website
As with any new technology, telehealth opportunities and challenges exist.
One of the biggest limitations of telehealth services is the digital divide. While 94.6% of Americans have internet access in 2024, not everyone will benefit equally from telehealth.
In lower-income areas, adoption rates are slower, possibly because people lack the necessary technology or because local healthcare providers aren’t offering virtual options.
Another concern is that as technology evolves, some patients, particularly older adults or those in vulnerable situations, might struggle to keep up. They could find themselves left behind, unable to access the services designed to help them.
There’s another big concern – the rising healthcare prices.
While virtual care and telehealth promise to make healthcare more efficient and cost-effective for now, it is not without some concerns.
Namely, there’s a worry that, in some cases, patients might have a telehealth visit and then be referred for an in-person visit for the same issue. In other words, employers and employees could end up paying twice for essentially the same service.
Also, telehealth visits might lead to more prescriptions for things like expensive medical equipment or lab tests that wouldn’t have been ordered in an in-person visit.
Ultimately, while telehealth holds excellent promise, addressing these challenges is essential to ensuring it benefits all patients equally and sustainably.
As we navigate through 2024, many legislative changes are shaping the telehealth landscape.
At the federal level, the Centers for Medicare & Medicaid Services (CMS) will continue to allow telehealth services without restrictions on location until December 31, 2024.
Furthermore, the American Medical Association (AMA) supports a new law proposal called the CONNECT for Health Act of 2023, which aims to expand Medicare coverage for telehealth services and permanently establish the temporary rules from the pandemic.
However, for telehealth services to be integrated effectively, more impactful federal and state policies are needed, and many new laws are being discussed at the state level.
A crucial aspect is coverage parity, which means that if a service is covered for in-person visits, it must also be covered when provided via telehealth, as long as it meets the standard of care.
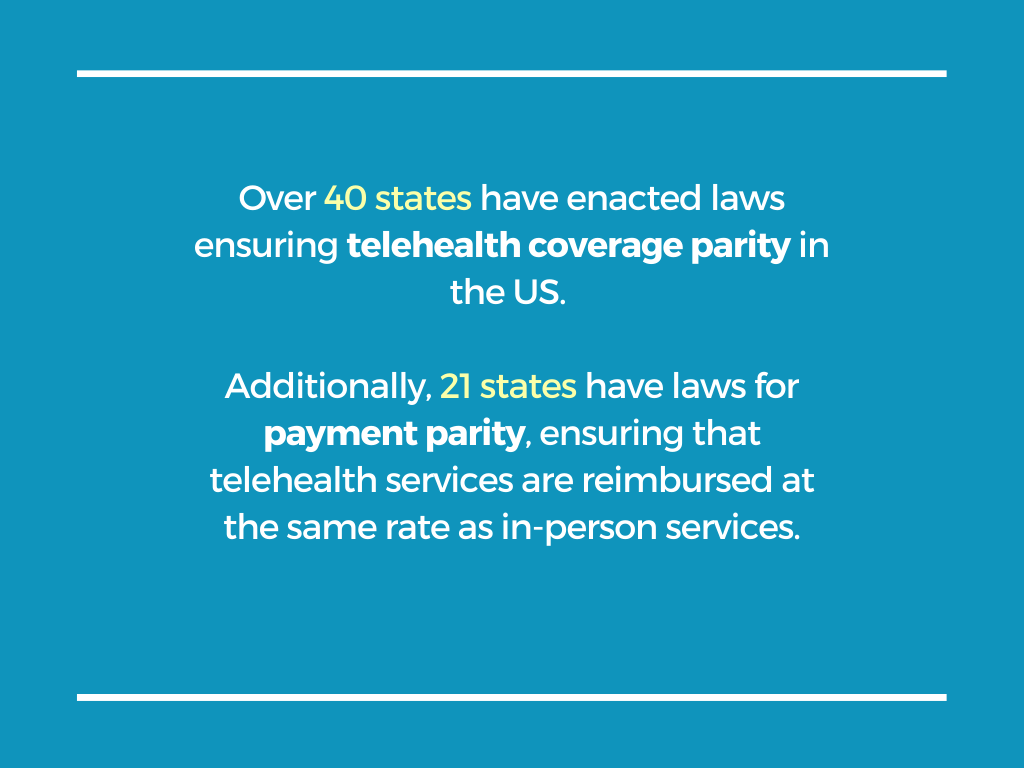
Today, over 40 states have enacted laws ensuring telehealth coverage parity.
Additionally, 21 states have laws in place for payment parity, ensuring that telehealth services are reimbursed at the same rate as in-person services.
All in all, the future of telehealth holds great promise. With these advancements in legislation, telehealth is bound to become a more integral part of healthcare delivery.
So, does telehealth reduce costs? The evidence suggests a resounding yes.
A wealth of data supports that telehealth visits cost less than in-person visits, with additional savings in indirect costs like travel and time off work. Furthermore, telehealth can prevent unnecessary ER visits and hospitalizations, leading to significant long-term cost reductions.
By making healthcare more accessible, convenient, and efficient, telehealth is not only reducing costs but also democratizing access to quality care for employees and providing substantial benefits for employers.
Disclosure: Some of the products featured in this blog post may come from our partners who compensate us. This might influence the selection of products we feature and their placement and presentation on the page. However, it does not impact our evaluations; our opinions are our own. The information provided in this post is for general informational purposes only.
Senior Content Writer at Shortlister
Browse our curated list of vendors to find the best solution for your needs.
Subscribe to our newsletter for the latest trends, expert tips, and workplace insights!
Discover 50+ essential infertility statistics and get valuable insights into this prevalent issue.
For countless employees in the United States, work is a source of physical discomfort and pain. How can corporate MSK programs help?

What compels someone to travel halfway around the world for a hip replacement or cancer therapy?

Workplace equity is more than a buzzword—it’s a lifeline in the fight against diabetes and the health gaps shaped by where we live, work, and grow.
Used by most of the top employee benefits consultants in the US, Shortlister is where you can find, research and select HR and benefits vendors for your clients.
Shortlister helps you reach your ideal prospects. Claim your free account to control your message and receive employer, consultant and health plan leads.